Ⅰ. Introduction
Mild Cognitive Impairment(MCI) is a deterioration in cognition greater than what is expected for a person’s age, but does not markedly interfere with daily activities. Out of 3% to 19% of MCI prevalence in those aged 65 or more, 20% to 46% develop Alzheimer's disease or dementia within 3 to 5 years(Ritchie, 2004; Tschanz et al., 2006). However, since 22% of MCI patients could be restored to normal cognitive function over time through early appropriate intervention, management of MCI has drawn much attention over the years(Ganguli, Dodge, Shen, & DeKosky, 2004).
MCI patients face problems with response to inhibition, switching, and cognitive flexibility, which are various aspects of executive functions compared with cognitively healthy elders(Law, Barnett, Tau, & Gray, 2011; Sanchez-Benavides et al., 2010; Traykov et al., 2007). Not only do tasks requiring executive function significantly affect those with MCI, it can also be reliable predictors of dementia before the diagnosis(Rapp & Reischies, 2005). In Marshall et al.(2011) study, examination of impairment in executive function across elderly with normal cognition to mild AD confirmed a strong relationship between executive dysfunction and IADL impairment. As executive dysfunction clearly impacts daily function in MCI clients, it is important to identify such individuals and provide quality treatment as early as possible. Treatments targeting executive dysfunction at early stages may further delay IADL impairment and improve patient’s quality of life.
Evidence for pharmacologic and non-pharmacologic treatments for individuals with MCI and dementia are currently being vigorously researched. Pharmacologic treatments use medication to slow the illness. However, there are only few medications that are approved to use due to difficulties, such as high cost of drug development and lengthy period of time needed to observe the effectiveness. Non-pharmacological therapies are an alternative treatment which aims to maintain or improve cognitive function, ability to perform ADL, improve overall quality of life, and/or reduce behavioral symptoms. Cognitive training in patients with MCI include cognitive restructuring, computer-assisted cognitive training, and relaxation to a group of MCI which resulted in an improvement of subjective memory(Rapp, Brenes, & Marsh, 2002; Rozzini et al., 2006).
Besides cognitive training, providing physical activity as an intervention for elderly at risk of dementia has shown to be an effective and costbeneficial way to both improve cognitive function and prevent MCI from progressing to dementia(Cui, Lin, Sheng, Zhang, & Cui, 2018). Lately, research on applying physical activity as interventions for MCI is actively encouraged. Systematic reviews on the effects of using physical activity as an intervention shows generally positive results in the overall cognitive domain(Ohman, Savikko, Strandberg, & Pitkala, 2014). However, there is a lack of evidence on the effects of physical activity in specific domains of cognition, such as executive function.
Thus, the aim of this paper is to systematically review the effectiveness of physical activity on executive functions of older adults with MCI. To understand the effect of physical activity on MCI compared to cognitive therapy, a popular treatment often delivered by occupational therapists, definition of physical activity is expanded to any intervention that was done in an active manner apart from table-top activities for this review.
Ⅱ. Methods
This systematic review is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis(PRISMA) guidelines (Moher, Liberati, Tetzlaff, & Altman, 2009).
1. Search strategy
The search was executed on April, 2018. The primary means of identifying studies to be included in this review was done through electronic search on PubMed, CINAHL, Medline, PsychINFO, Embase, and Cochrane databases. Search terms included “MCI” OR “mild cognitive impairment” AND “physical activit*” OR “physical performance” OR “physical exercise*”, AND “executive function*. Additional strategy included handsearching through previously published systematic reviews on physical exercise for the elderly, MCI, and dementia populations.
2. Eligibility criteria
Studies were eligible if they met the following inclusion criteria: 1) participants have a diagnosis of MCI and the criteria used for the diagnosis is clearly stated; 2) study is published in a peer- reviewed journal and conducted in a Randomized Controlled Trial(RCT) design; 3) interventions must include physical activity delivered in forms of exercise and/or leisure; and 4) outcome measures must include at least one executive function measure that is clearly identified by the author as a measure used to examine executive function. Studies were excluded if they were: 1) prospective or retrospective cohort studies; 2) case reports or cross-sectional studies; 3) grey literature, such as conference abstracts or protocols; or 4) not written in English.
3. Study selection
Two stages of screening were conducted: stage 1—title/abstract screening and stage 2—full text screening. During stage 1, titles and abstracts of retrieved articles were examined through EndNote X8.2 by two independent reviewers(first and second authors), and both exclusion and inclusion criteria were applied. Consensus was reached through discussion.
For stage 2, full-length articles were re-examined and ultimately selected according to the eligibility criteria. This was also done independently by two same reviewers. An excel sheet was created to keep record of reasons for accepting and rejecting articles as well as extracting information to be analyzed.
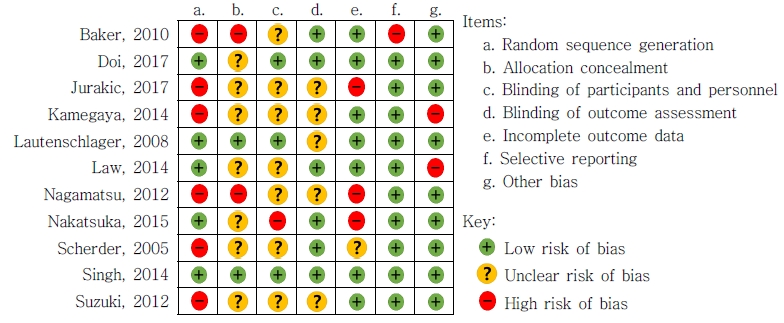
4. Risk of bias assessment
Even though RCTs that are appropriately conducted minimize confounding factors and bias, when it is not appropriately done, it may result in biased interpretation of the results. Therefore, it is imperative to consider risk of bias in RCTs when reviewing the evidence.
The Cochrane Collaboration’s tool for assessing risk of bias was used to measure risk of bias in selected articles. Physiotherapy Evidence Database (PEDro) scale, which is widely used especially when evaluating risk of bias in therapeutic studies, was not selected for this review. As the items in the scale do not weigh the same and should not be summed up to obtain a total quality score, Cochrane Collaboration’s tool was a better selection to assess each bias one by one for this review(Higgins & Altman, 2008).
The seven domains that were reported as risk of bias include selection bias in random sequence generation, selection bias in allocation concealment, performance bias, detection bias, attrition bias, reporting bias, and other bias(Higgins et al., 2011). Each domain was rated as low, high, or unclear by two independent researchers. The two researchers practiced assessing risk of bias on an unrelated article to confirm the understanding of assessment. Differences in outcome were discussed together until consensus was reached.
Ⅲ. Results
1. Study selection
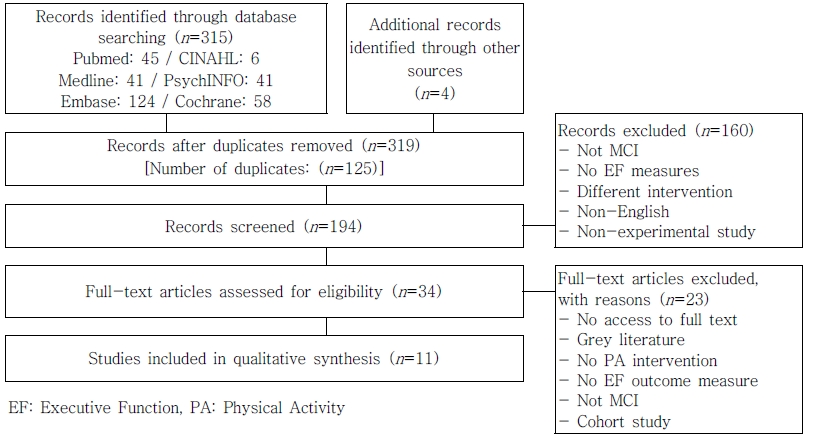
Eleven studies that met the eligibility criteria were selected. Initially, 315 studies were retrieved through PubMed, CINHAL, Medline, PsychINFO, Embase, and Cochrane databases. Four additional studies were identified through hand-searching and included for the selection process. Using EndNote, two researchers independently removed 125 duplicates after consensus leaving 139 studies for screening.
After reviewing the title and abstract according to the inclusion and exclusion criteria, 34 studies were left. A total of 160 studies that did not meet the eligibility criteria were excluded. Reasons behind exclusion are not including MCI participants; having no executive function measures; using interventions other than physical activity; articles written in foreign language; and non-experimental studies.
Full-text review of the remaining 34 studies were done by the two researchers in the same manner, and 11 studies were ultimately selected. Studies that were excluded after reading full-text include having no access to full article; being in a form of grey literature; having no physical activity intervention, executive function outcome, and/or MCI participants; and being a cohort study(Figure 1).
2. Participant characteristics
The mean age of the participants ranged from 68 to 82 with the most participants in 70 to 75 years of age. As for gender distribution of the participants, out of 11 studies, five studies had relatively balanced number of males and females while four had more females than males and two consisted only females. Six studies provided mean Mini- Mental State Examination(MMSE) scores, which ranged from 22.2 to 27.9 out of 30, as the baseline cognition. Two studies used Montreal Cognitive Assessment(MoCA; range 22-26 out of 30, lower score indicates greater cognitive impairment) and two Alzheimer Disease Assessment Scale-Cognitive Subscale(ADAS-Cog; range 7-8.79 out of 70, higher score indicates greater cognitive impairment). One study provided a shortened version of MMSE, 12-item MMSE(range 9.23-9.83 out of 12, lower score indicates greater cognitive impairment), as the general cognition baseline. Overall, general cognitive score of all participants were in a score range indicative of mild cognitive impairment, regardless of being in the intervention or control group(Refer to Appendix 1 for information on the characteristics of selected studies).
3. Intervention characteristics
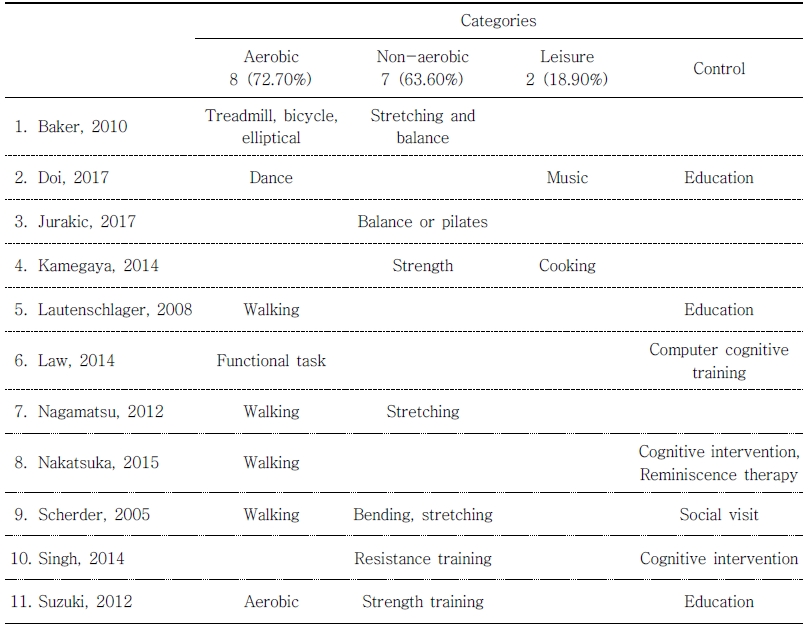
All studies disclosed operational definitions of intervention programs and its counterparts. Intervention characteristics were classified into three main categories: aerobic, non-aerobic, and leisure. Aerobic category included dancing, walking, and using treadmill, bicycle, or elliptical. Nonaerobic category included stretching, balancing, and strength training, such as resistance training and core exercises. Music program consisting of playing instruments and leisure activities, such as cooking, handcrafts, and competitive games were considered as a leisure category. Intervention for the control group consisted of providing healthrelated education, cognitive training through computer program or reminiscence therapy, and social visits (Table 1).
Three studies explored the effect of multicomponent interventions(Kamegaya, Araki, Kigure, Long- Term-Care Prevention Team of Maebashi City, & Yamaguchi, 2014; Singh et al., 2014; Suzuki et al., 2012). Multicomponent interventions were comprised of a combination of non-aerobic component with aerobic, leisure, or control, such as education.
As for mode of delivery, seven studies offered intervention in a group form. Two studies provided individual intervention and the other two studies were conducted in a combination of group and individual(Appendix 1).
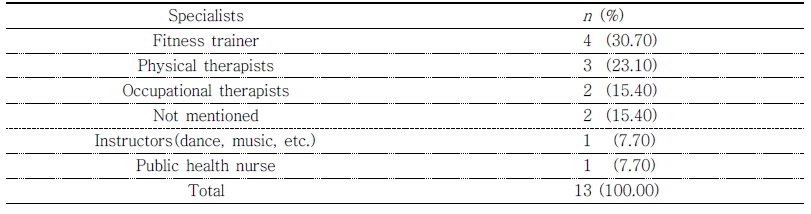
Out of 11 studies, four involved fitness trainers to provide intervention regarding aerobic and non-aerobic components. For three studies, physical therapists lead both aerobic and non-aerobic components. Occupational therapists delivered aerobic and leisure components as intervention in two studies. There were one instructor and one public health nurse who were each involved in a separate intervention. Two studies did not identify the specialist providing the intervention. As Kamegaya et al.(2014) used a group of healthcare professionals- an occupational therapist, a physical therapist, and a public health nurse, the sum of the specialist exceeds 11(Table 2).
4. Dependent variable analysis
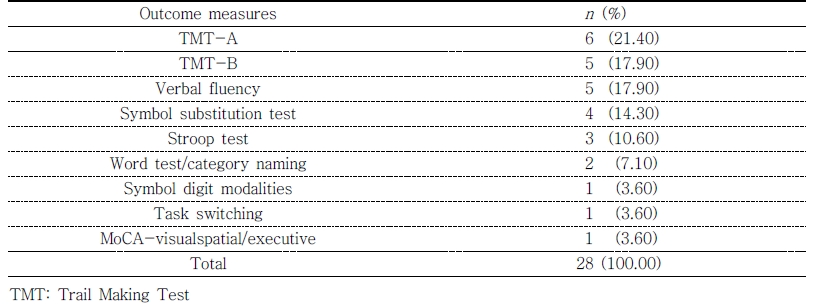
For each of 11 studies analyzed in this study, dependent variables that evaluated the executive function were examined. One or more of following seven outcome measures were used to evaluate executive function in each study. The most frequently used assessment tools were Trail Making Test (TMT)-A and TMT-B used in six(21.40%) and five(17.90%) studies, respectively, and Verbal Fluency used in five studies(17.90%). Symbol Substitution Test was used in four studies(14.30%) followed by Stroop Test in three studies(7.10%) and Word Test/Category Naming in two studies (7.10%). Symbol Digit Modalities, Task Switching, MoCA-visualspatial/executive was used only once in the selected studies(Table 3).
5. Risk of bias within studies
The Cochrane Collaboration’s Tool for assessing risk of bias rates each study as having 1) low risk of bias, 2) unclear risk of bias, or 3) high risk of bias. Among the selected studies, there were three that showed low risk of bias for almost all items (Doi et al., 2007; Lautenschlager et al., 2008; Singh et al., 2014). On the other hand, four studies were found to have high and/or unclear risk of bias in more than half of the items(Baker et al., 2010; Jurakic, Krizanic, Sarabon, & Markovic, 2017; Kamegaya et al., 2014; Nagamatsu, Handy, Hsu, Voss, & Liu-Ambrose, 2012). The eleven studies selected for the review showed differences in risk of bias to a varying degree(Table 4). As metaanalysis conducted on a group of study with heterogeneity may lead to differences in observed effects, meta-analysis was not performed in this study(Haidich, 2010).
Ⅳ. Discussion
This systematic review examined the effect of physical activity interventions on executive function for older adults with MCI. Eleven RCTs published between 2005 to 2017 were included in the analysis.
Out of the selected studies, eight showed promising results while one had mixed results and two ineffective. To further analyze the results, physical activities were grouped into three categories: aerobic, non-aerobic, and leisure. Positive change in executive function for aerobic and non-aerobic categories were observed(Baker et al., 2010; Jurakic et al., 2017; Law, Barnett, Yau, & Gray, 2014; Nagamatsu et al., 2012; Scherder et al., 2005). However, two studies involving aerobic and leisure activities showed no change in executive function compared to the control group, which received education(Doi et al., 2017; Lautenschlager et al., 2008). Rest of the studies involving aerobic components generated positive change in executive function, which is in line with previous research on aerobic exercise training associated with modest improvements in attention, processing speed, executive function, and memory(Smith et al., 2010).
Three studies provided multicomponent programs by combining non-aerobic component with aerobic, leisure, or cognitive activities. All studies involving multicomponent programs yielded positive effects on executive function(Kamegaya et al., 2014; Singh et al., 2014; Suzuki et al., 2012). This may be due to the nature of executive function. As executive function encompasses various cognitive abilities, such as decision making, planning, self-monitoring, behavior initiation, organization, and inhibition, it may be best approached with multicomponent interventions.
In spite of promising results, three studies showed no difference in change of executive function between intervention and control groups after the treatment(Doi et al., 2017; Lautenschlager et al., 2008; Nakatsuka et al., 2015). There were no characteristic differences, such as participant age, gender distribution, baseline cognition, and mode and duration of intervention delivery. However, these three studies tended to have larger number of sample size compared to other studies. Sample size ranged from 45 to 85 when other studies ranged from 10 to 43.
The intervention programs were provided mostly by fitness trainers followed by physical therapists and occupational therapists. Regardless of intervention components, physical activity interventions provided by physical therapists and occupational therapists showed positive effects on executive function in MCI. Physical therapists are more equip to provide treatment that enhance physical and functional abilities, while occupational therapists have advanced understanding of complexities of intertwined physical and cognitive components and provide meaningful tasks for interventions(AOTA, 2018; APTA, 2018). The lack of explanation on how specialists managed interventions and how participant adherence was sustained may contribute to the conflicting results.
The strength of this study is the high level of evidence for therapeutic studies achieved by conducting a systematic review of RCTs. According to the levels developed by the Centre for Evidence Based Medicine(CEBM; 2009) for treatment, this study analyzed individual RCT(second highest level: 1B) and produced a systematic review (highest level: 1A). Moreover, the selected studies were conducted fairly recently spanning from 2005 to 2017, with more than half of the studies published in the last 5 years. Focusing on a specific cognitive domain(executive function) to specific intervention(physical activity) provides an opportunity to take a closer look at the effect on each other in MCI population.
There are some limitations to the current study. The selected studies were conducted in a wide variety of countries. Although this contributes valuable information on how providing physical activity as an intervention for MCI population is of interest globally, cultural differences provide limitations to applying the intervention. Careful consideration before implementing the program is necessary.
Only two out of eleven studies involved occupational therapists when providing interventions. There is a lack of quantitative evidence for occupational therapists to provide physical activity for MCI participants to examine their change in executive function. More studies involving occupational therapists when providing physical activity to MCI clients need to be examined to confirm consistent findings.
For future practice and research implications, occupational therapists can refer to this review to plan for intervention targeting executive function of MCI clients, and the effect of their intervention can in turn add to the evidence. Furthermore, collection of individual participant data or aggregate data from the studies listed above for a meta-analysis is a possible area of research to examine the overall effect of the intervention. If both published and unpublished results including positive and negative outcomes of the relevant studies are used for meta-analyses, the effect of physical activity on executive function of older adults with mild cognitive impairment will be better understood.
Ⅴ. Conclusion
Beneficial effects of various physical activity interventions on executive functions of MCI participants have been observed in the majority of selected RCT studies. However, some studies show contrasting results which complicate interpretation of the results. To thoroughly understand the effect of physical activity on executive function in older adults with MCI, physical activity along with cognitive approach in the field of occupational therapy needs to be actively explored.