Ⅰ. Literature Review
Postpartum Depression(PPD) affects women after childbirth. In the United States, PPD affects one in nine women, with a prevalence as high as one in five women in certain states(Center for Disease Control and Prevention, 2017). Symptoms, including exhaustion, anxiety, and extreme sadness, are persistent and severe, and commonly emerge in the first week to month postpartum(National Institute of Mental Health, n.d.). Some women also experience anger and worry that they will hurt their babies. Common treatments for PPD include medications and psychotherapy.
Many women fear taking antidepressants, or any medications, in the postpartum period. Medications can pose risks to the infants if the drug is present in high enough levels in breastmilk. A 2011 study (Berle & Spigset, 2011) indicated that some antidepressants are safe to take while breastfeeding, while other medications leave detectable levels of the drug in the infant’s blood. Cost of medication also serves as a barrier to a client’s adherence to an antidepressant medication routine(O’Donohue & Levensky, 2006). In addition, the perceived stigma associated with taking antidepressants is enough to deter some from seeking pharmacological treatment (Sirey et al., 2001). As an adjunct to medications or to avoid the potentially harmful effects of antidepressants on the infant, among other barriers to medication adherence, women are seeking nonpharmacological approaches to treat PPD.
McCurdy, Boule, Sivak, & Davenport(2017) conducted a meta-analysis on the effects of a nonmedical intervention, light-to-moderate exercises (including yoga, aerobic exercise, resistance training, whole body stretching), in reducing depressive symptoms postpartum. This review compared 16 articles and found strong support for light-tomoderate exercise being effective in reducing depressive symptoms. The evidence indicated that exercise improved the woman’s odds of resolving depressive symptoms by 54.00%, among other health benefits. McCloskey and Reno(2019) conducted a systematic review on the effects of complementary health approaches, including yoga, aromatherapy, infant massage, mindfulness training, bright light therapy, and supplements, in reducing postpartum depressive symptoms. This review compared 10 articles and found moderate support to indicate that complementary health approaches are effective in reducing depressive symptoms. Both articles support the use of non-pharmacological interventions as effective treatment options for PPD.
Occupational therapists promote participation in daily living through engagement in meaningful activities. This occupational participation improves overall mental health(AOTA, 2016). The American Occupational Therapy Association’s (AOTA) Vision 2025 identifies women’s health as an emerging occupational therapy practice area(AOTA, 2018). In efforts to address the needs of this population, the AOTA also established a Women’s Health Community of Practice as a Special Interest Section on their 2018 plan(AOTA, 2019).
This systematic review seeks to examine the evidence for the efficacy of non-medical interventions for women with PPD within the scope of occupational therapy, specifically yoga, social support groups, and kangaroo care. These three non-medical interventions have been most frequently studied among potential non-medical interventions that could be utilized by occupational therapists for PPD. No other systematic reviews comparing these topics were found during the literature review.
Ⅱ. Methods
Researchers searched the key databases CINAHL, Cochrane Library, PubMed, and Scopus. The following key words were used during the database searches: kangaroo care, depression, postpartum, kangaroo-mother care method, postpartum depression, skin-to-skin, yoga, support group, and perinatal depression. In determining which studies to include, the following criteria were developed: discussed both the intervention(or alternate, equivalent terms) and postpartum depression(or alternate, equivalent terms) or maternal mood postpartum; was published during the years 2000 to 2018; was peer-reviewed, available in full text, and was available in English. Articles were excluded if they did not meet the inclusion criteria, were dissertations or theses, were below a Level II evidence according to the standards set by Sackett, Rosenberg, Muir Gray, Haynes, & Richardson(1996), were retrospective studies, focused on the effect of intervention on the infant, or analyzed any intervention other than those listed (i.e. CBT, massage, music therapy). Articles were also excluded if they focused on breastfeeding outcomes, focused on the father, did not include any intervention strategies, focused on parent-infant relationships, focused on prevention, included diagnoses other than postpartum depression (i.e. anxiety, PTSD, low mood), or if the support group was an online support or focused on partner support. Initial searches yielded 75 articles. After screening, the researchers assessed 31 full-text articles for eligibility, and screened eligible articles based on inclusion criteria, with collaboration from faculty mentor. 13 articles met inclusion criteria, as depicted in Figure 1. Other reasons for exclusion were that the articles focused on the father, breastfeeding outcomes, focused on prevention, and/or included any other diagnoses than PPD. Upon selecting articles, materials were then categorized by levels of evidence according to the American Occupational Therapy Association(AOTA, 2017) Guidelines for Systematic Reviews, and then evaluated for risk of biases (Higgins, Altman, & Sterne, 2011).
Ⅲ. Results
Thirteen studies were assessed to evaluate the effects of interventions on postpartum depression. The interventions were divided into three types: kangaroo care(four articles), yoga(five articles), and social support groups(four articles). The articles consisted of six articles of Level I evidence and seven articles of Level II evidence (Armstrong & Edwards, 2004; Bershadksy, Trumpfheller, Kimble, Pipaloff, & Yim, 2014; Bigelow, Power, MacLellan- Peters, Alex, & McDonald, 2012; Buttner, Brock, O’Hara, & Stuart, 2015; Castral et al., 2014; Field, Diego, Delgado, & Medina, 2013; Chen, Tseng, Chou, & Wang, 2000; Gjerdingen, McGovern, Pratt, Johnson, & Crow, 2013; Herizchi, Hosseini, & Ghoreishizadeh, 2017; Holditch-Davis, White-Traut, Levy, & O’Shea, 2014; Ko, Yang, Fang, Lee, & Lin, 2013; Prevatt, Lowder, & Desmarais, 2018; Reid, Glazener, Murray, & Taylor, 2002). To quantitatively assess the effectiveness of interventions on postpartum depression, six articles used the Edinburg Postpartum Depression Scale(EPDS), six used the Center for Epidemiological Studies-Depression Scale(CES-D), two used the Beck Depression Inventory(BDI), one used the Structured Clinical Interview Depression (SCID), one used the Profile of Mood States(POMS), two used the Patient Health Questionnaire(PHQ), one used the Hamilton Depressive Rating Scale(HDRS), one used the Inventory of Depression and Anxiety Symptoms (IDAS), two used the Medical Outcomes Study 36-Item Short Form Health Survey(SF-36), one used the Health Related Quality of Life(HRQoL), one used the Perceived Stress Scale(PSS), one used the State Anxiety Inventory(STAI), one used the State Anger Inventory(STAXI), and one used the Inter-personal Support Evaluation List(ISEL). Several studies used more than one inventory to measure depressive symptoms.
Each intervention strategy was assessed individually and collectively to examine how depressive symptoms improved for those involved in treatment. When the articles were examined to understand the overall effects of interventions on postpartum depression, 11 studies found statistically significant results, found in Table 1(Armstrong & Edwards, 2004; Bershadksy et al., 2014; Bigelow et al., 2012; Buttner et al., 2015; Castral et al., 2014; Chen et al., 2000; Field et al., 2013; Herizchi et al., 2017; Holditch-Davis et al., 2014; Ko et al., 2013; Prevatt, Lowder, & Desmarais, 2018). Two additional articles found clinically meaningful results, while the results did not reach statistical significance(Gjerdingen et al., 2013; Reid et al., 2002).
1. Yoga
Five articles examined yoga as an intervention strategy for postpartum depression. Yoga interventions ranged from eight to twelve weeks in duration, and individual session lengths ranged from 45 minute to 90 minute sessions. Two studies compared the effects of the yoga intervention group with control mothers in a social support group. Both studies found significantly higher reductions in depressive symptoms for mothers who participated in yoga compared to mothers who participated in social support groups(Armstrong & Edwards, 2004; Field et al., 2013). Three studies also found significant reductions in depressive symptoms in women who participated in yoga when compared to scores on depression inventories for women who did not participate in yoga interventions(Bershadksy et al., 2014; Buttner et al., 2015; Ko et al., 2013).
2. Kangaroo care
Four articles examined kangaroo care as an intervention strategy for postpartum depression. Results of all four studies indicated statistically significant declines in depressive symptoms of mothers who performed kangaroo care postpartum (Bigelow et al., 2012; Castral et al., 2014; Herizchi et al., 2017; Holditch-Davis et al., 2014). Two articles found that the positive effects of kangaroo care were sustained over a period of time, noting significant reductions in depressive scores at one month postpartum(Bigelow et al., 2012; Herizchi et al., 2017). Multisensory intervention in NICU involving kangaroo care(Holditch-Davis et al., 2014), One article examined depressive symptoms at a specific point in time(Castral et al., 2014). Other articles examined depressive symptoms over the course of the first month of the infant’s life. These two studies found that control group mothers showed increases in depressive symptoms at one month postpartum, compared to mothers who participated in kangaroo care(Bigelow et al., 2012; Herizchi et al., 2017).
1) Social Support Groups
Four articles examined social support groups as an intervention strategy for postpartum depression. Social support interventions included attendance of weekly peer-support groups either in person or via telephone. All four articles found that social support groups reduced depressive symptoms in women postpartum(Chen et al., 2000; Gjerdingen et al., 2013; Prevatt et al., 2018; Reid et al., 2002). However, two articles did not find statistically significant differences in depressive symptoms of intervention mothers compared to control group mothers; however, these women still experienced reductions in scores on depression inventories administered, indicating a potential for clinically meaningful results to support the use of social support groups as effective interventions for PPD(Gjerdingen et al., 2013; Reid et al., 2002). One study indicated the social support group intervention was effective in reducing depressive symptoms of women who experienced an unplanned Cesarean section. These results are noteworthy as this specific population of postpartum women are at higher risk for PPD(Prevatt et al., 2018).
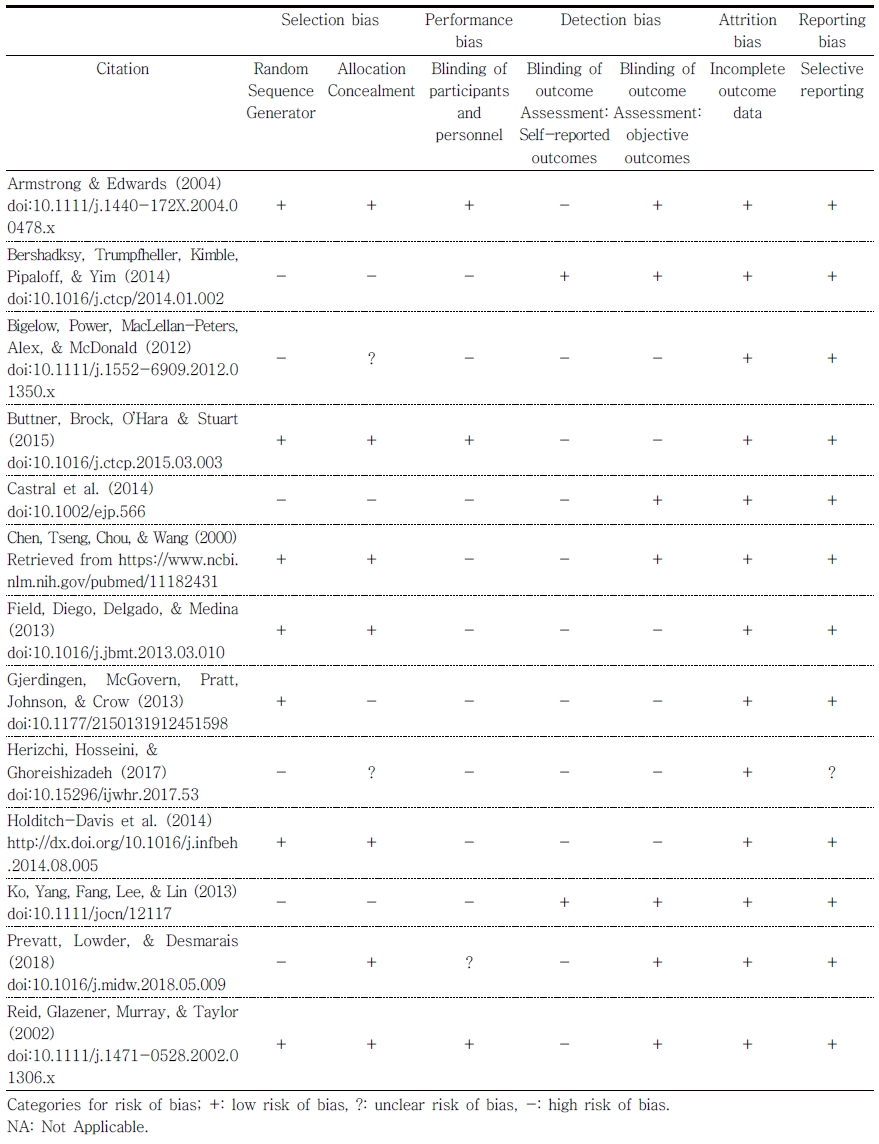
2) Risk of Bias
All 13 articles in this systematic review were evaluated for risk of selection bias, performance bias, detection bias, attrition bias, and reporting bias via methods outlined by Higgins et al.(2011). As depicted in Table 2, seven articles showed evidence for random allocation sequence generation. Allocation concealment was reported in seven articles. Performance bias was a high risk in nine studies. There was low risk of attrition bias in all 13 articles. Reporting bias was unclear in one article, and low risk in the remaining 12 articles. Biases in the articles resulted from a variety of factors: some studies used convenience sampling; researchers could not deny a mother from participating in alternate forms of intervention that may have interfered with improved outcomes in depressive symptoms; all measures of depression and quality of life are self-reported measures.
Ⅳ. Discussion
The purpose of this systematic review was to examine the efficacy of non-medical interventions in women with PPD. Non-medical interventions examined were kangaroo care, yoga, and social support groups. Thirteen articles were evaluated. Of these articles, six were Level I evidence and seven were Level II. The outcome of the review showed strong evidence to support yoga, moderate evidence to support kangaroo care, and moderate evidence to support social support groups as effective interventions in reducing depressive symptoms in women postpartum.
The strong evidence supporting yoga as an effective intervention in reducing postpartum depressive symptoms also indicated yoga as more effective than social support groups alone in achieving the desired effects. Moderate evidence supported kangaroo care as an effective intervention in reducing postpartum depressive symptoms. Moderate evidence also supported social support groups as an effective intervention in reducing postpartum depressive symptoms. Also, in studies that compared yoga interventions to social support group interventions, yoga was significantly more effective in reducing symptoms of postpartum depression.
Strengths of the review include the exhaustive search of multiple databases that was conducted and the high levels of evidence for the comprehensive set of articles collected. Limitations of the review include only articles for which full publications were available in English were considered and few high-level articles exist on other non-medical interventions, narrowing the focus of the review. Also, performance bias was high in the majority of the studies(nine studies). This review could be strengthened by evaluating and including evidence for additional interventions for PPD so that non-medical interventions in addition to yoga, kangaroo care, and social support groups could be used in occupational therapy practice.
The findings of the review have the following implications for OT:
Occupational therapy is expanding services to include involvement in women’s health and perinatal care, taking a health promotion approach. Practitioners in the NICU, pediatrics, and primary care who work with pregnant or postpartum women can also recommend yoga, social support groups, and kangaroo care to women with PPD to ease the transition to motherhood.
OT education is needed to increase awareness of PPD and suggest potential intervention strategies that therapists can utilize for treatment sessions with new mothers.
Occupational therapists who practice or have an interest in OT in Women’s Health can join the AOTA Community of Practice for Women’s Health to connect with other professionals and advocate for expansion of practice areas to include Women’s Health.
Further research is needed to assess nonmedical interventions with PPD. These studies should be of high levels of evidence to increase strength of findings.
Ⅴ. Conclusion
This systematic review examined the efficacy of specific non-medical interventions for women with PPD. The purpose was to understand the effectiveness of kangaroo care, yoga, and social support groups to reduce postpartum depressive symptoms to evaluate the benefits of their use in occupational therapy interventions. The review found strong evidence to support the use of yoga, moderate evidence to support the use of kangaroo care, and moderate evidence to support the use of social support groups to decrease depressive symptoms in postpartum women. This suggests that non-medical interventions are effective in reducing PPD symptoms and should be implemented in occupational therapy sessions to maximize treatment outcomes and improve depressive symptoms and occupational participation in postpartum women. Future research should include the systematic evaluation of the effectiveness of other nonmedical interventions for PPD(i.e. massage, relaxation techniques, light therapy, music therapy). Research should also explore the effectiveness of OT in reducing depressive symptoms with this population as well as the role of occupational therapy in women’s health, in general, especially within the context of psychosocial interventions that implement preventative coping strategies with perinatal women. Occupational therapists can utilize these findings by recommending and utilizing alternative non-medical interventions for women with postpartum depression in efforts to contribute to this emerging societal need.