Ⅰ. Introduction
Primary care is an emerging practice area for Occupational Therapists (OTs). OTs have a unique skill set allowing them to address the multi-faceted needs of patients (Mackenzie et al., 2018). As patients in a primary care setting require integrated and holistic care, OTs enable patients to actively participate in personal goal setting allowing patients the onus to self-manage their own health and well-being (Bolt, Ikking, Baaijen, & Saenger, 2019). OTs can address chronic illness and geriatric syndromes through all types of prevention. Geriatric syndromes include conditions that are related to aging (Guaraldi, 2016). These conditions include falls, frailty, dementia, depression, delirium, incontinence, vertigo, osteoporosis, failure to thrive, and polypharmacy (Guaraldi, 2016). Falls are often the costliest of the geriatric syndromes causing both physical and mental harm to those who experience them (Boyd & Stevens, 2009).
Over 8 million United States (US) emergency room visits per year result from falls, comprising more than 20% of overall hospital visits National Floor and Safety, 2017). Each year over 3 million adults report at least one fall in a 90-day period (Boyd & Stevens, 2009). Falls are a known issue for the aging population, as each year approximately one-fourth of people aged 75 and older experience two or more falls typically occurring during self-care or Activities of Daily Living (ADLs) and functional mobility (walking, transfers, etc.) (Abdelrahman & Elawam, 2014; Shumway-Cook et al., 2009). Although a fall may be an isolated incident, recurrent falls can lead to more serious consequences (Abdelrahman & Elawam, 2014). Compared to a solitary fall, recurrent falls typically lead to more complicated injuries and time in the hospital resulting in higher medical costs and institutionalization (Abdelrahman & Elawam, 2014; Shumway-Cook et al., 2009). OTs are essential to providing effective and occupation-based fall prevention interventions within primary care and throughout the continuum of care (Mackenzie et al., 2018). OTs offer education on fall prevention, screen for likelihood of falls, and provide education and physical activity interventions to prevent recurrent falls (Mackenzie et al., 2018).
As Human Immunodeficiency Virus (HIV) has progressed to a chronic disease, People Living With HIV (PLWH) tend to experience many common age-related co-morbidities including diabetes, heart disease, osteoporosis, kidney disease, respiratory diseases and physical dysfunction including falls (Guaraldi, 2016). PLWH have an amplified burden of age-related comorbidities in comparison to individuals who are not infected by HIV (Guaraldi, 2016; Guaraldi et al., 2011). PLWH show signs of age-related comorbidities, such as frailty, falls, delirium, and incontinence earlier than do those without HIV (Bielderman et al., 2013; Guaraldi, 2016; Ruiz, Reske, Cefalu, & Estrada, 2013; Zhang, Guo, Gu, & Zhao, 2018). Frailty is clinically measured using the Clinical Frailty Scale and Fried’s modified criteria (CFS) (Fried, Ferrucci, Darer, Williamson, & Anderson, 2004; Rockwood et al., 2005; Zhang et al., 2018). Fried et al. (2004) characterized frailty using five symptoms: weight loss, weakness, exhaustion, slow functional mobility, and decreased physical activity. Another common characteristic of aging is urinary incontinence or unintentional urine release (Soliman, Meyer, & Baum, 2016). The need to void urine frequently or urgently and the sensation of unintentionally releasing urine can lead people to move quickly and unsafely to the restroom resulting in a fall (Soliman et al., 2016).
Although the presentation of frailty and incontinence appear to have some connection to unanticipated falls, the effect these phenomena have on aging PLWH lacks correlative evidence. As a result, no occupation-based interventions address frailty and incontinence among PLWH. The objective of this case-control study was to examine the relationship of frailty, incontinence and falls among PLWH in Houston, TX. These analyses explored two hypotheses. First, we hypothesized that PLWH who are frail will have an increased likelihood of falling when compared to PLWH who are not frail. Second, we hypothesized that PLWH who are incontinent will have an increased likelihood of falling compared to PLWH who are continent. The research team hypothesized that comorbid conditions including cardiovascular disease, balance deficits, visual impairments, weight loss, and the demographic variables of gender, age, and insurance status, would correlate with falls among PLWH (Meir-Shafrir & Pollack, 2012). These analyses offer a better understanding of possible risk factors for falls among PLWH to devise occupational therapy interventions to reduce the likelihood of fall-related injuries.
Ⅱ. Methods
1. Study Design
Our analyses used a retrospective case-control design with non-matched controls. Data were extracted from Electronic Medical Records (EMR) of PLWH who had received hospital-based occupational therapy services in Houston, TX, from May 2015 to May 2017. Research protocols were reviewed and approved by the institutional review boards of University of Texas Health Science Center at Houston and Houston Methodist Hospital Institutional Review Boards and the large academic hospital that provided the data for the study. To ensure reliability of the sample, the hospital’s research office selected a sample of the data and double-entered it into the database to confirm that data were collected accurately. The final data set was de-identified and provided to the research team for analysis.
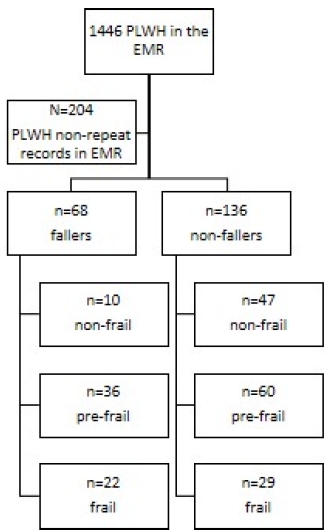
A total of 1446 records were extracted from the EMR. Of these, 1242 did not meet inclusion criteria resulting in 204 unduplicated records. Of the 204 participants included in the final dataset, 68 were identified as cases because they reported experiencing a fall within 12 months of admission. The remaining 136 were identified as controls because they had not reported experiencing a fall during that timeframe (Figure 1 and Figure 2). Inclusion criteria for the cases included: (1) documentation of HIV-positive status in the EMR; (2) Aged >18 years at the time of admission; (Centers for Disease Control, 2017) experiencing a fall within12 months of hospital admission; and (4) evaluation/treatment from occupational therapy. Controls were PLWH who received occupational therapy but who had not sustained a fall in 12 months prior to admission. Exclusion criteria for both cases and controls were an incomplete medical record which included missing data such as age, race, lab values, etc.
2. Measures
1) Falls
Falls, the outcome variable of interest, was created by categorizing PLWH whose self-reported medical record indicated he or she experienced a fall 12 months prior to admission. Those who reported a fall were coded as fallers.
2) Frailty
We created a categorical variable to identify the level of frailty among participants. These categories for frailty include weight loss, weakness, exhaustion, slow functional mobility, and decreased physical activity (Fried et al., 2004). PLWH who satisfy none of the criteria were considered non-frail, PLWH who satisfy 1-2 criteria were classified as pre-frail, and PLWH who fulfilled 3 or more criteria were classified as frail (Bieniek, Wilczyński, & Szewieczek, 2016; Fried et al., 2004). Only a final score for frailty was extracted from the EMR resulting in our inability to calculate a measure of internal reliability. In general-population samples, the CFS was found to have good reliability (α=0.95) (Zhang et al., 2018).
3) Incontinence
We created a dichotomous variable to identify participants who were incontinent. PLWH who reported the unintentional loss of urine on more than one occasion in the past 12 months were categorized as incontinent (Brown, Vittinghoff, & Wyman, 2000; Hung et al., 2017).
4) Demographic characteristics
Age of participants was recorded as a continuous variable while gender (male, female), insurance coverage type: private or Medicare (yes, no), and having Medicaid (yes, no) were recorded as categorical variables. Having access to health insurance has been associated with reducing the risk factors leading to falls as people with insurance tend to utilize healthcare when necessary (AOTA, 2010; Bresnick, 2017).
5) Comorbid diagnoses
Cardiovascular disease was defined as an array of conditions that affect the heart including blood vessel diseases, arrhythmias, congenital heart defects, atherosclerosis, angina, heart attack, and stroke (Meir-Shafrir & Pollack, 2012).Balance disturbances were measured using Berg Balance Scale during occupational therapy evaluations (Berg, Wood- Dauphine, Williams, & Gayton, 1992). Because only final scores were extracted from the medical record, we did not calculate a measure of internal reliability. In other samples, the scale has good internal reliability (α=0.77) (Berg et al., 1992). Visual impairments were defined as severe reduction in vision and decreases a person’s capacity to perform tasks (Lord, Smith, & Menant, 2010; Pathai, Deshpande, Gilbert, & Lawn, 2009). Based on data in participants’ medical record, dichotomous variables were created for cardiovascular disease, balance deficits, and visual impairments. A categorical variable was created for Body Mass Index (BMI) through dummy coding the variables with a BMI less than 18.5 were coded as underweight, those with a BMI of 18.5-24.9 were coded as normal and those with a BMI of 25 or greater were coded as overweight (Keys, Fidanza, Karvonen, Kimura, & Taylor, 1972).
3. Data Analysis
We analyzed the data separately to test the different hypotheses. Initially, we analyzed the data comparing how the presentation of all three categories of frailty related to falls among PLWH. For the continuous variable age, we performed a student’s t-test. We performed chi-square test of homogeneity on categorical variables, the comorbidities of note, to describe both the fallers and non-fallers in this group. The association between potential risk factors, the co-morbidities, along with the categories of frailty and falls was quantified by the odds ratio (OR) and its 95% confidence interval (CI). Variables significant at the bivariate level (p<0.2) were entered a multivariate logistic regression model used to estimate the odds of falling based on demographic characteristics and known comorbidities. We decided to place the variables that were significant at the 0.20 level or lower due to wanting to explore alternative strategies to determining significance and our low sample size (Vakhitova & Alston-Knox, 2018). Stata 14 was used for all statistical analysis (StataCorps, 2017).
Ⅲ. Results
The overall sample characteristics and results of bivariate analyses are summarized in Table 1. Our analyses found that age was not statistically significant; however, the ages of our population was young for a falls study. The average age of participants who were coded as fallers was 50 (+11.50) years, while the average age of non-fallers was 52 (+10.80) years.
The majority of our sample who were male (77.94%), categorized as pre-frail (52.94%) or frail (32.35%), and had balance deficits (57.35%) experienced falls. We performed two regression models. In our first Multivariate Logistic Regression model (MLR), we were interested in understanding the association between frailty and falls among PLWH. We entered variables significant at p<0.20 at the bivariate level into the multivariate model. The first MLR model (Table 2) measured the association between frailty and falls among PLWH. In this text, the Odds Ratio (OR) can be found in parentheses. The 95% confidence intervals (CI) are indicated in brackets. Participants with a pre-frail diagnosis were over twice as likely to fall as non-frail participants (OR=2.77 [1.18-6.52]). Please see Table 2 for the results of the multivariable regression.
Table 2
Adjusted Logistic Regression of Frailty and Factors Associated With Falls (Non-Fallers and Fallers) N=204

|
In the second multivariate model (Table 3), we found that our variable urinary incontinence (OR=1.38 [.60-3.22]) was not statistically significant. Due to the shared covariance between incontinence and other variables. Due to the collinearity issue with the variable of incontinence, we were unable to make a reliable claim that incontinence is correlated with falls in this sample.
Table 3
Adjusted Logistic Regression of Incontinence and Factors Associated With Falls (Non-Fallers and Fallers) N=204

|
For the sake of science, we performed an MLR with the variables of incontinence as well as the three categories of frailty to examine how the independent variables impacted falls together. Those participants who were not frail was less likely to fall (p=0.035). All other results lacked statistical significance.
Ⅳ. Discussion
Our analysis suggests that PLWH who presented as pre-frail were more likely to fall than PLWH who were non-frail. Less than 20% PLWH were non-frail and experienced a fall, while greater than 50% and almost a third of the PLWH who pre-frail and frail were experienced a fall respectively. Similar results have been reported in other studies. For example, a large study involving older community-dwelling women revealed that frailty was a significant indicator for falls (Ensrud, Ewing, & Taylor, 2007). This study found that the relationship between frailty criteria and falls demonstrated that women in the pre-frail group were 1.23 times more likely to fall or have a recurrent fall than non-frail women (OR=1.23; [.02-1.48]) and women in the frail group were 2.41 times more likely to fall than non-frail women (OR= 2.41; [1.93-3.01]) (Ensrud et al., 2007). Another study found that men and women who were classified as frail were greater than 3 times more likely to fall than non-frail adults (Nelson, Dufraux, & Cook, 2007; Nowak & Hubbard, 2009). In all, PLWH who are pre-frail or frail appear to be more likely to fall than persons who are non-frail. As a result, screening for frailty during primary care visits with occupational therapy and offering education and occupation-based interventions may reduce the likelihood of falls.
Our analysis demonstrates that PLWH are more prone to fall at a younger age than the general population. Throughout the literature on frailty and falls, participants are aged > 60 years (Ensrud et al., 2007; Nelson et al., 2007; Nowak & Hubbard, 2009). However, our analysis found that PLWH are falling as early as aged 26 years of age. As a result, assessing frailty at occupational therapy visits within primary care from initial diagnosis can reduce the both the physical and economic impact of frailty on PLWH. Once assessed, addressing frailty through occupation-based interventions can reduce the physical, psychological, and economic costs of frailty and improve health outcomes for PLWH (Muldoon, 2017).
Our analysis contributes to the current literature by offering evidence that rehabilitating PLWH with pre-frail and frail conditions may reduce falls. As OTs are beginning to practice in primary care, addressing geriatric syndromes prior to their presentation may positively improve health outcomes and overall well-being among PLWH. In addition, the results of our analysis suggest that a further examination of pre-frail and frail conditions among PLWH may improve health outcomes of PLWH when paired with occupation-based interventions to reduce the likelihood of falls in this population. This phenomenon has not been studied by OTs due to chronic HIV’s lack of public presencea and interest in the last few years. HIV is now a chronic disease, which should make OTs more interested in treating PLWH.
By using occupation-based interventions aimed at addressing the factors leading to frailty, occupational therapists can decrease hospital admissions and secure suitable and safe discharges back into the community for the pre-frail and frail population of PLWH (College of Occupational Therapists, 2016; Muldoon, 2017). Occupational therapists offer direct attention to a person’s important occupations ensuring successful participation in ADLs and improving quality of life (Muldoon, 2017). For example, one study found that the discipline of occupational therapy was the lone hospital expenditure with which supplementary spending had a statistically significant link with decreased readmission rates for the three common health disorders of heart failure, pneumonia, and acute myocardial infarction (Rogers, Bai, Lavin, & Anderson, 2016). These three health conditions are linked to frailty in the aging population and PLWH (Weiss, 2011). Rogers et al. (2016) found that occupational therapy brings attention to issues connected to hospital readmission rates such as decreasing barriers in a client’s environment. OTs use occupation-based interventions to provide family/ caregiver training, provide home safety assessments and interventions, provide education and training on the use of adaptive equipment and durable medical equipment, and offer guidance for the subsequent levels of care for any patient admitted into the hospital (Rogers et al., 2016).
Our results reveal a correlation, although not statistically significant, between incontinence and falls, among PLWH highlighting another connection that has not been previously examined in the rehabilitation literature related to PLWH. In future studies, a larger sample might demonstrate a stronger correlation between incontinence and falls among PLWH. Despite this lack of significance at the multivariate level, the results of our study suggest that a further examination of treatments and prevention of incontinence among PLWH might improve positive health outcomes when combined with occupation-based interventions. OTs assist with bladder and bowel management of their patients. As toileting and toilet hygiene are ADLs, OTs have evidenced-based occupation-based strategies to assist with the management of continence and an overall reduction of costs associated with frailty and incontinence leading to improved health care outcomes and reduced spending for insurance companies, PLWH, and caregivers.
Impairments in balance are known causes of falls (Erlandson et al., 2012; Erlandson et al., 2016). The prevalence of balance deficits in this study population was 38.73% (Berner, Morris, Baumeister, & Louw, 2017; Erlandson et al., 2016). Through observation and clinical practice, addressing balance issues will reduce the likelihood of falls in PLWH. Our analysis found that balance, when entered the multiple regression model, may contribute to the number of falls among PLWH which may lead to increased likelihood of falls. Occupational therapists address balance deficits with occupation-based interventions aimed at improving physical function such as increasing core strength, increasing independence with functional mobility using appropriate durable medical equipment, teaching balance strategies, and adapting physical environments to account for balance issues.
Falls themselves may lead to serious bodily injury or bed-ridden status causing muscle atrophy and reduction of core strength leading to subsequent falls (Richert et al., 2014). In addition, musculoskeletal strength declines in aging populations leading to an increase in the likelihood of falls (Richert et al., 2014). As PLWH have an accelerating aging process, these individuals now have an earlier onset of age-related concerns including physical and psychological issues (Richert et al., 2014). Based on the literature, falls can lead to poor health outcomes for PLWH (Hunter & Kearney, 2018; Richert et al., 2014). These poor outcomes can lead to decreased quality of life and other psychological issues (Richert et al., 2014). In general, OT-based studies typically have fewer than 50 participants (Hunter & Kearney, 2018). These studies often use pre/posttest designs, systematic reviews, or are case studies aimed at an intervention or condition (Hunter & Kearney, 2018). Few OT studies involved more than 200 participants, use a case-control design and none have examined falls among PLWH.
Several limitations exist to this study. Casecontrol studies are subject to selection and observation bias. We had access to only one of many hospitals in the Texas Medical center resulting in a decrease in generalizability in our findings to all PLWH. The sample size was small compared to typical case-control studies found in falls literature (Hunter & Kearney, 2018). For example, our 1 case to 2 controls ratio was determined based on the current literature of studies involving falls, recurrent falls, and risk factors (Joosten, Demuynck, Detroyer, & Milisen, 2014). Since we had access to more data, we oversampled to achieve greater power for an n=204; 68 cases and 136 controls. Despite the sample being large for a traditional OT study, our sample size is considered small. In addition, falls recorded in the medical record are based on patients’ self-report meaning PLWH may be under or over-reporting the occurrence of falls (Cummings, Nevitt, & Kidd, 1988; Freiberger & de Vreede, 2011; Ganz, Higashi, & Rubenstein, 2005). As with most case-control studies, this study can only recognize this relationship but not establish a causal relationship. Despite these limitations, we collected comprehensive data, including demographic, medical record and functional assessment data, to categorize the risk factors for falls.
Many risk factors for falls have been identified before; however, little information examining PLWH who have had some type of OT were known. Therefore, the outcomes of this analysis warrant further research considerations to assist in the prevention of falls among PLWH. The presentation of frailty criteria, gender, lack of insurance coverage, and balance deficits were independently associated factors for falls in this population. In the present analysis, a causal relationship between frailty, gender, insurance coverage, balance, and falls is not yet clear. Therefore, further prospective study involving this population would be beneficial and necessary.
Further study in this population using a longitudinal cohort approach may provide better evidencedbased interventions improved health outcomes for PLWH. This type of study would involve following PLWH over time to discover if modifying the effects of frailty and incontinence using occupation-based interventions would decrease the likelihood of falls and reduce overall health costs while improving quality of life.
Ⅴ. Conclusions
Our analysis offers an opportunity for further study of evidenced-based OT-interventions to reduce falls in PLWH. From the data gathered in this study, PLWH fall at earlier ages than in the general population. In addition, pre-frail and frail conditions are indicators of falls in this population. Using occupation-based interventions, occupational therapist can provide environmental modifications, adaptive equipment and durable medical equipment recommendations to reduce the likelihood of falls and assist with the management of frailty among PLWH. In addition, this analysis offers occupational therapists an opportunity to use prevention skills to screen for frailty earlier, to reduce the number of readmissions into the hospital based on frailty and falls among PLWH. Further, ensuring that occupational therapists address balance deficits as part of the evaluation and plan of care for PLWH may reduce falls and hospital readmission rates for PLWH. Addressing balance problems should lead to better functional mobility. Falls can be prevented using education, screening for fall risk, frailty, and balance deficits, and improving the mobility of PLWH. Community dwelling as well as hospitalized PLWH who are pre-frail or frail and have balance issues may experience an increase in the likelihood of falls. Clinicians should be conscious of the morbidity issues associated with falls to best combat fall risk. Further study is required to gain an enhanced understanding of how frailty affects PLWH. Using evidenced-based interventions aimed at reducing the effects of frailty among PLWH, clinicians and researchers can reduce the likelihood of falls among PLWH. The results obtained from this analysis support the necessity for early screening for fall risk in PLWH.