Ⅰ. Introduction
Health-Related Quality of Life (HRQOL) is a construct of quality of life relevant to health (Crosby, Kolotkin, & Williams, 2003). HRQOL can be measured via self-perceived interpretation of one’s health status and overall well-being, in relation to personal expectations (internal attributes), culture and values (external attributes) (Crosby et al., 2003). Approximately 10 years ago, selfreported or person-centered outcome measures were unique and started to become increasingly important type of outcome variable (de Wit & Hajos, 2013). This is because stakeholders could gain different information about individuals who medically have similar information (share the same diagnosis), however report having different subjective views of their own health and wellbeing. Thus, these types of assessments began being integrated into health care systems like Inpatient Rehabilitation Facilities (IRF) and used with stroke survivors to determine patient-centered goals, treatment successes and clinically important differences (Algurén, Fridlund, Cieza, Sunnerhagen, & Christenssor, 2012; Sabogal, Vidal, Pedraza, Sanchez-Pedreno, & Guevara, 2016; Lin, Fu, Wu, & Hsieh, 2011). Even clinical trials were incorporating patient reported outcomes including HRQOL to evaluate the effectiveness of treatments (US Department of Health and Human Services Food and Drug Administration, 2014).
The majority of research studies on HRQOL are with the well elderly population who are aging (Khaje-Bishak, Payahoo, Pourghasem, & Jafarabadi, 2014; Baernholdt, Hinton, Yan, Rose, & Mattos, 2012; Garcia & Navarro, 2018). A longitudinal study of aging non-institutionalized adults compared to people with various longstanding illnesses, determined that limitations in mobility and difficulties with everyday activities were negatively impacting quality of life for both groups (Netuveli, Wiggins, Hildon, Montgomery, & Blane, 2006). More recently, an investigation of HRQOL with stroke survivors reported worst quality of life especially for those who lived alone (Haley, Rother, Kissela, Perkins, & Howard, 2011). Another study determined lower HRQOL overtime for both stroke caregivers as well as the person experiencing the stroke (Carod- Artal & Egido, 2009).
The EuroQoL 5-Dimensions Questionnaire (EQ-5D) is a generic HRQOL assessment that has strong psychometric properties and includes an overall index score as well as a visual analog scale of wellbeing (VAS) (Dorman, Waddell, Slattery, Dennis, & Sandercock, 1997). A recent study tested the five-level version of the EQ-5D’s validity, responsiveness, and minimal clinically important difference in stroke patients undergoing rehabilitation (Chen et al., 2016). The results of this study were fair to good concurrent validity depending on the measure of comparison (r=.255, -.703, p<.05), fair predictive validity with all measures including the FIM (r=-.027, p<.05) and moderate responsiveness to change (SRM=0.63) (Chen et al., 2016). Approximately 33.8% of study participants exceeded the minimal clinically important difference values based on the approach used (Chen et al., 2016). There are a few articles on the strong reliability of the EQ-5D, with the stroke population (Dorman et al., 1997; Golicki et al., 2015; Hunger, Sabariego, Stollenwerk, Cieza, & Leidl, 2012). The test-retest reliability of the EQ-5D was also found to be good, however psychological function (anxiety/depression) was the most limited of the domains (Dorman, Slattery, Farrell, Dennis, & Sandercock, 1998). Also, good interobserver agreement (k>.0.60) was found for all dimensions of the EQ-5D (Pinto, Maso, Vilela, Santos, & Oliveira-Filho, 2011).
This current study was interested in retrospectively reviewing clinical data on the EQ-5D administered in an IRF with stroke survivors. We used aspects of the Chen et al. 2016 article to guide our objectives however we were using classic threelevel version of the EQ-5D. Psychometric properties were tested for the classic three-level version however not using the Functional Independence Measure (FIM) as the comparison measure within 6 months post-stroke (Hunger et al., 2012). It appears that functional independence may be directly related to high HRQOL because disability was found to be a negative determinant of HRQOL (Carod-Artal & Egido, 2009). The FIM is collected routinely with all patients at IRFs to estimate functional independence. Thus, the first objective of this study was to describe the study participants, by characteristic and demographic variables. The second study objective was to examine the relationship between HRQOL and function independence, using the EQ-5D compared to the FIM at admission and discharge. The third objective was to determine the impact of standard therapy on HRQOL on EQ-5D (both the index score and VAS). We hypothesize the group to be diverse group of stroke survivors. Also, that there will be a strong correlation between these two measures in this patient population because of the relatable constructs of function. Furthermore, we hypothesize the participants will have improved HRQOL index score and improved health status on the VAS, overtime.
Ⅱ. Methods
1. Procedures
This study was approved by the Institutional Review Board (IRB) at Kessler Foundation in West Orange, New Jersey. This approval included a waiver for data use (IRB #: E-828-14). EQ-5D implementation started as a quality improvement project within the therapy department at the IRF three years prior to the initiation of this retrospective study. It was common that the management at this hospital would implement specific outcome measures to be trialed as part of standard care. The process to implementing a new measure would start with an in-service to all staff members. Management would share information about why the outcome measure was going to be part of their required work. Then, training on how to use the outcome measure would take place. This usually was done in another in-service (Santana et al., 2015). After the outcome measure was being used clinically, staff would be notified that occasional audits would be completed by management in order to ensure compliance. The final step would involve management consulting with the quality improvement team in order to determine whether the assessment was able to capture the necessary information or show change. For this initiative, the EQ-5D and the FIM were required to be administered to all stroke patients within 72 hours of admission and discharge from the IRF. These outcome measures were administered by speech, physical and occupational therapists.
2. Participants
For the purposes of this retrospective study, we used specific inclusion criteria based on the research question. Thus, the data included participants who met the following inclusion criteria: (1) diagnosis of stroke via medical records, (2) verbally able to communicate without difficulty and (3) cognitively intact. The exclusion criteria were: (1) any other diagnosis or condition other than stroke, (2) any type of aphasia, and (3) cognitive deficits. The reason we excluded people with aphasic as well as those with impaired cognition is because these individuals had EQ-5D scores were missing from our chart review. After investigating why the assessment scores were missing, it was determined that the clinical notes referred to aphasia and/or impaired cognition limiting the persons’ ability to provide a self-report.
3. Study Variables
1) Demographic or characteristic variables.
The demographic and characteristic variables for this group included gender, ethnicity, age, Length of Stay (LOS), and discharge disposition. These data were found in the patients’ individual medical record.
2) EuroQol 5-Dimensions Questionnaire (EQ-5D)
There are 5 dimensions of this scale (Dolan, 1997). They include mobility, self-care, usual activity, pain/discomfort and depression/anxiety. Each of the dimension items are scored on a Likert scale. There are 3 response options to measure HRQOL. A score of 1 is no problems, score of 2 is moderate problems, or a score of 3 is extreme problems. Thus, the higher the score, the more independent the person is on this scale. To calculate the EQ-5D weighted index, we used the values set by Shaw, Johnson, and Coons (2005) and converted the five dimensions into a single score. There is a VAS that is part of the EQ-5D, which is a scale like a thermometer that ranges from endpoints of 0 or worst imaginable health to 100 or best imaginable health status. The person is to rate their health by placing an “X” on the thermometer scale. The numerical score is then determined based on the location of where the “X” was placed. The scale has strong psychometric properties established in the stroke population including the minimal important difference range (Kim, Kim, Jo, & Lee, 2015).
3) Functional Independence Measure (FIM)
The most common measure of the burden of care related to motor and cognitive function is an assessment called the FIM, which consists of 18 items. Thirteen items are assessing motor function. These include eating, grooming, bathing, upper body dressing, lower body dressing, toileting, bladder management, bowel management, bed/chair/ wheelchair transfer, toilet transfer, tub/shower transfer, walk/wheelchair mobility, and stairs. The 5 items that are of the cognitive domain are comprehension, expression, social interaction, problem solving and memory. Each item is scored on a scale from 1-7 (with 7 as independent and 1 is total assistance). The range of the total motor FIM score is 13 to 91 points and range for cognition is 5 to 35. The higher the score, the more independent the person (Ottenbacher, Hsu, Grager, & Fiedler, 1996).
4. Data Analysis
The EQ-5D and FIM scores were entered into the electronic medical record system by the therapists administering the assessments. After study approval, we then imported the scores and other study variables into the statistical software program. All analyses were completed using SPSS 25®. Normal distribution was checked for each variable before analysis and no heteroscedasticity was found nor any violations of normality and linearity. Descriptive statistics were completed on all study participants. Pearson’s correlation was used to conduct a correlation between the EQ-5D (index score only) and the FIM, two separate times at admission and then again for discharge scores. A paired-samples t-test was conducted to evaluate the impact of standard therapy on HRQOL on EQ-5D (both the index scores and VAS). Effect size or the ratio between the mean change scores and the standard deviation of the baseline scores was calculated. The range used for interpretation was .02-.04 (small effect), 0.5-.06 (medium effect) and .07-.09 (large effect) (Kazis, Anderson, & Meenan, 1989). Statistical significance was determined using p<.05 for all analyses.
Ⅲ. Results
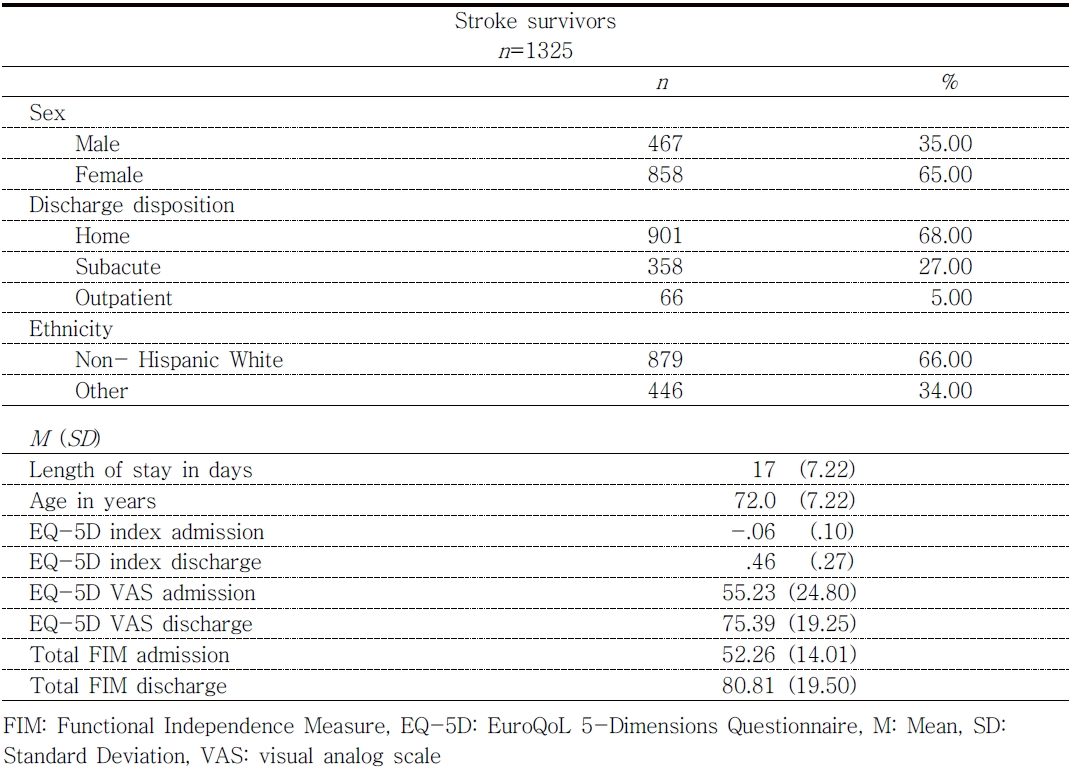
The EQ-5D was administered to a total of 1527 stroke survivors during the clinical implementation. For the study analysis, there were 202 stroke survivors excluded. Of the 202, 181 (89.8 %) were excluded because that did not have a true stroke after completing the retrospective chart review. The other 21 (10.2%) were excluded because they could not answer the EQ-5D questions independently due to cognition or aphasia. The final number of study participants included in the analysis was n=1325. This group consisted of mostly white (66%), females (65%), a mean age of 72 years (SD=13.28) and average LOS in the IRF of 17 days (SD=7.22). See Table 1 for additional demographic, participant characteristic data and mean scores for the FIM and EQ-5D.
The relationship between the EQ-5D and FIM was investigated using Pearson’s correlation coefficient. There was a weak, positive correlation found between the two variables at admission (r=.15, n=1325, p<.000). Similar findings from a separate analysis were found for the discharge scores (r=.04, n=1325, p<.000).
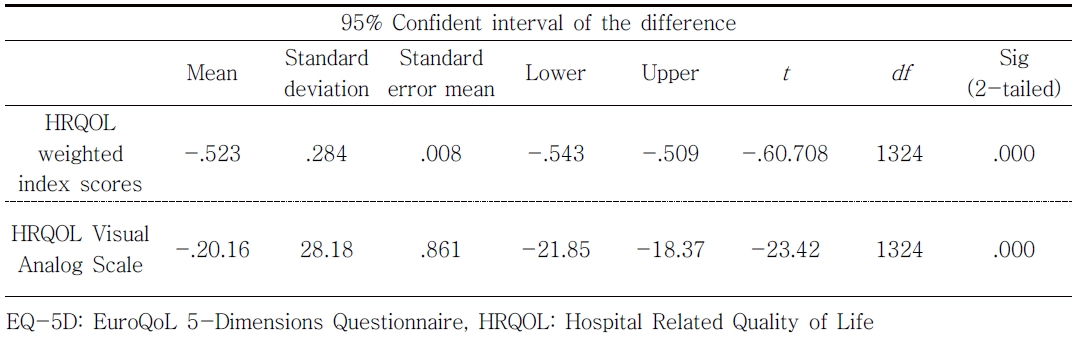
A paired-samples t-test revealed a statistically significant increase in HRQOL index scores from admission (M=-.06, SD=.10) to discharge [M=.46, SD=.27, t(1324)=-60.71, p<.000]. For the VAS, the paired-samples t-test revealed a statistically significant increase from admission (M=55.23, SD=24.80) to discharge [M=75.39, SD=19.25, t(1324)=-23.42, p<.000]. See Table 1 and 2 for these data. Also, the eta squared statistics (.74 and .70) indicated a large effect size, respectively. The mean weighted score of .52 was determined to be higher than the established range of .27- .50, for the minimally important difference.
Ⅳ. Discussion
This clinical initiative implemented a patientreported HRQOL, the EQ-5D, in a group of stroke survivors in IRF. There have been initiatives similar to this study to support patient engagement through use of patient-reported outcomes (Santana et al., 2015). The retrospective study first determined descriptively that the data included a large group of stroke survivors, mostly older, Caucasian women who were discharged home at the end of their IRF stay. These results as well as the feasibility of implementing this measure is similar to the EQ-5D study that was completed in Germany (Hunger et al., 2012).
Next, the results indicated a weak relationship was present between HRQOL and function, suggest these assessments should be used independent of each other. This finding did not support our hypothesis or the findings of Carod-Artal & Egido (2009) study that found disability to be a negative determinant of HRQOL. However, Chen et al. (2016) conclusion of excellent concurrent validity with the FIM and index scores, supported the important role of functional independence correlating with HRQOL.
Finally, a statistically significant change in addition to large effect sizes in both the index and VAS scores suggests improvement in HRQOL overtime with standard care. This finding is different from Hunger et al. (2012) however similar to Golicki et al. (2015) where they did find the scale captured change overtime. This finding supports the importance of using a patient-reported outcome measure in IRF to capture what the person believes their own health status to be. Occupational therapists and other health care professionals should be intentional about understanding the patients’ view especially when it can assist with goal setting for therapy.
A strength of this study is the large sample however because the data was not originally collected for research purpose thus, there were limitations to what data was available and the overall study design. Another study limitation is that our sample may not have been representative of all stroke survivors undergoing rehabilitation because we excluded charts at the time of analysis. There was not a control group thus limiting the interpretation of the findings. Lastly, since the FIM is not an assessment that is used worldwide to measure functional independence and because it was replaced on October 1, 2019 with another functional coding system, future studies should replicate and verify these findings using the new measure (Centers for Medicare and Medicaid Services [CMS], 2018).
Ⅴ. Conclusion
In conclusion, EQ-5D is an outcome measure that healthcare professionals, like occupational therapists, can use to assess HRQOL with stroke survivors to capture the patient’s perspective of this important construct. This retrospective study also contributes to the discussion of the relationship between HRQOL and functional independence, which we conclude as being independent of each other. Also, this study provides initial data to suggest further research be conducted to better understand the impact of standard care on HRQOL.