Ⅰ. Introduction
Adverse Childhood Experiences (ACEs) are defined as traumatic incidents experienced before 18 years of age (Centers for Disease Control and Prevention, 2019). According to the National Child Abuse and Neglect Data System, 12.5% of all US children have had a documented episode of child abuse or neglect reported by the age of eighteen (Wildeman et al., 2014). The World Health Organization reported from 22% to 76% of children being physically abused in countries around the world (WHO, 2017). ACEs increase the likelihood of physical and mental health problems including learning problems, greater use of health and mental health services, greater involvement with child welfare and juvenile justice systems, and chronic health problems (Anda et al., 2006). Exposure to abuse increases the risk for emotional and behavioral complications, including depression, anxiety, Post-Traumatic Stress Disorder (PTSD), dissociation, impaired self-esteem, delinquency, bullying, and self-harming thoughts, which lead to poor social and developmental outcomes (Melville, Kellogg, Perez, & Lukefahr, 2014; Okada et al., 2018). Such disturbances in lifestyle patterns have long-term effects on health and quality of life. Interventions are inadequate and evidence-based practices continue to be sparse, particularly regarding sleep interventions for children with ACEs (Shipman & Taussig, 2009).
Sleep is paramount to proper health, development, and cognitive functioning across the lifespan. An estimated 25-40% of children and adolescents experience sleep disturbances (Meltzer & Mindell, 2006). The impact of sleep deprivation ranges widely, influencing cognition, social functioning, academic performance, and emotional regulation. Sleep disturbances can translate into difficulties with cognitive flexibility, reasoning, planning, and impulse control (Peach & Gaultney, 2013). Problems with sleep have been shown to weaken the neuronal connection between the frontal cortex and the amygdala. Decreased use of this circuit can lead to difficulties in emotional regulation (van der Helm, Gujar, & Walker, 2010). Additionally, sleep is a significant predictor and antecedent of neurodevelopmental and mental disorders, such as depression (Carskadon et al., 2012; Sadeh, Tikotzky, & Kahn, 2014). The mental health impact of sleep problems manifests itself in children with symptoms, such as PTSD (Demirci, 2018; Hambrick, Rubens, Brawner, & Taussing, 2018; Melville et al., 2014; Schneiderman, Susman, & Negriff, 2018), psychological distress (McPhie, Weiss, & Wekerle, 2014, Mignot et al., 2018; Schneiderman et al., 2018; Yen, Ko, Liu, & Hu, 2015), dissociation (Hébert, Langevin, Guidi, Bernard- Bonnin, & Allard-Dansereau, 2017; Melville et al., 2014), mental disorders and suicidality (Mansbach- Kleinfeld, Ifranh, Apter, & Farbstein, 2015; Okada et al., 2018; Yen et al., 2015), and self-blame and self-injurious thoughts (Melville et al., 2014).
Understanding the relationship between trauma and sleep is important to better guide occupational therapists assessment and intervention for children. The American Occupational Therapy Association (AOTA, 2019) has recognized Children and Youth as an important emerging practice area in the 21st century. In 2008, the AOTA recognized sleep as an occupation and it is now included in the Occupational Therapy (OT) domain (AOTA, 2014). Decrease in sleep quality negatively impacts a person’s quality of life and occupational performance, engagement, and participation in daily activities. Intervention studies have demonstrated occupational therapy’s effectiveness in addressing sleep dysfunction for older adults and children with autism or attention deficit/hyperactivity disorder (Gregory, Morgan, & Lynall, 2012; Ismael, Lawson, & Hartwell, 2018; Koenig & Rudney, 2010; Leland et al., 2016; Vasak, Williamson, Garden, & Zwicker, 2015). However, it has been noted that occupational therapy practitioners lack adequate training to treat sleep problems and, thus, are not prepared to screen for factors affecting sleep participation or offer skilled services to improve the quality of sleep (Ho & Siu, 2018; Leland et al., 2014; Tester & Foss, 2018). The objectives of this study were to explain the relationship between traumatic events and sleep problems in children and discuss the clinical implications of results for the field of occupational therapy.
Ⅱ. Methods
An exhaustive literature search was performed on sleep quality in children who had experienced adverse events by the research team with help from the librarians at the University of Texas Medical Branch. The formal research question was are adverse childhood experiences related to quality of sleep in children?
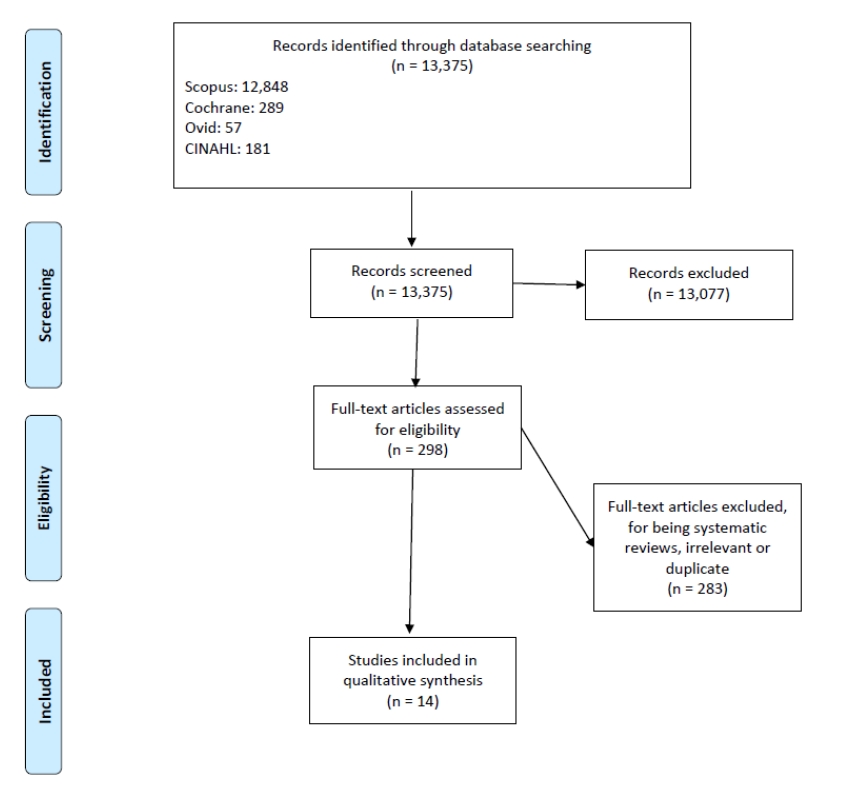
The search was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines from the American Occupational Therapy Association (AOTA, 2020). Records were identified through PubMed, CINAHL, Scopus, and Ovid. The researchers collaborated on setting inclusion and exclusion criteria and assessed each article for appropriateness before including it in the final systematic review. The search strategy was adapted to fit the parameters of each database but generally followed the approach outlined below.
Search terms focused on sleep, trauma, and child identifiers for all four databases. Included articles represented a level of evidence above Level 4 (see Table 1), included studies comparing trauma and sleep, were available as full-text and in English, were published in the last five years (2014-2019), and covered a participant population age of 0-18 years for the review to focus on children only (Tomlin & Borgetto, 2011). Articles were excluded if they represented a level of evidence that was less than Level 3, were not available as full-text or in English, were not current literature (published before 2014), included study participants who were older than 18 years, or were not relevant to the review’s research question. Levels of evidence were determined based on the PRISMA guidelines from the American Occupational Therapy Association (AOTA, 2020). See Table 1 for details. Articles that matched the inclusion criteria and appropriately addressed the research question were further assessed for eligibility. Included articles were agreed upon by all members of the research team. All included articles and risk of bias values were reviewed by at least two team members. Ongoing and completed systematic reviews addressing the relationship between sleep and trauma in children were screened in the Cochrane, PROSPERO, and the aforementioned databases to avoid duplication of past or current literature. Figure 1 depicts the flow of the article decision process.
Table 1
Levels of Evidence
Ⅲ. Results
The present review sought to examine the relationship between trauma and quality of sleep in children, which led to the final review of 14 qualified articles. These studies included 2,596,118 participants from eight countries. Four studies were conducted in the United States (Hambrick et al., 2018; Hash et al., 2019; Melville et al., 2014; Schneiderman et al., 2018), three in Canada (Hébert et al., 2017; Langevin, Hébert, Guidi, Bernard-Bonnin, & Allard-Dansereau, 2017; McPhie et al., 2014), two in Taiwan (Wang, Raffeld, Slopen, Hale, & Dunn, 2016; Yen et al., 2015), one in Brazil (Fontes, Conceição, & Machado, 2017), one in France (Mignot et al., 2018), one in Israel (Mansbach-Kleinfeld et al., 2015), one in Japan (Okada et al., 2018), and one in Turkey (Demirci, 2018). No Level 1 or 2 studies met the inclusion criteria of this review since they did not involve experimental components. All 14 studies were Level 3B. Article types are denoted in Table 2.
Table 2
Evidence Table
[i] ACEs: Adverse Childhood Experiences, AIS-8: Athens Insomnia Scale, CDI: Children’s Depression Inventory, CPS: Childhood Protective Services, CSA: Child Sexual Abuse, C-SBEQ: Chinese version of the School Bullying Experience Questionnaire, DAWBA: Development and Well-Being Assessment, ETQT: Exit Telephone Questionnaire for Therapists, ITQT: Initial Telephone Questionnaire for Therapists, K-SADS-E: Kiddie-Schedule for Affective Disorders and Schizophrenia, M: Mean, MAP: Maltreatment and Adolescent Pathway, MASC-T: Taiwanese version of the Multidimensional Anxiety Scale for Children, MC-CES-D: Mandarin Chinese version of the Center for Epidemiological Studies-Depression Scale, NCS-A: National Comorbidity Survey Replication Adolescent Supplement, PeNSE: National School Health Survey-Pesquisa Nacional de Saúde do Escolar, PFR: Promoting First Relationships, R & R: resource and referral, RSES: Rosenberg Self-Esteem Scale, SDQ: Strengths and Difficulties Questionnaire, YSSC: Youth Symptom Survey Checklist
In all of the 14 articles in this review, a negative association was found between trauma and childhood sleep disturbances for children from as young as 10 months to as old as 18 years. When comparing the sleep quality of children who have been maltreated versus not maltreated, children who have been abused experience significantly greater problems with sleep than children who have not been abused (Langevin, Cossette, & Hébert, 2016). One study found differences between sexes and did not find a relationship for males between maltreatment and sleep disturbances nor PTSD symptoms and sleep disturbances (Schneiderman et al., 2018). The reviewed studies were categorized by (1) age of participants, (2) research design, (3) type of trauma experienced by participants, (4) outcome measures, and (5) description of sleep problems.
1. Risk of bias
Each study was individually assessed by pairs of reviewers for risk of bias on a scale of low, high, or unclear based on the Cochrane Handbook for Systematic Reviews of Interventions (Higgins, Altman, & Sterne, 2011). All studies were identified as having a high risk of selection bias, performance bias, and detection bias as their methods mentioned no use of random sequence generation, allocation concealment, or blinding. See Table 6 for details about Risk of Bias.
2. Age
This review included articles that involved children from 0-18 years old. Of the 14 studies, only one examined infant and toddler participants (0-2 years old) (Hash et al., 2019). Three included participants in the 2-11 year old age range (Hébert et al., 2017; Langevin et al., 2017; Okada et al., 2018). Ten included participants in the adolescent age range (12-17 years) (Demirci, 2018; Fontes et al., 2017; Hambrick et al., 2018; Mansbach-Kleinfeld et al., 2015; McPhie et al., 2014; Melville et al., 2014; Mignot et al., 2018; Schneiderman et al., 2018; Wang et al., 2016; Yen et al., 2015).
3. Control group
Of the 14 studies reviewed, five incorporated a control group design. The control groups varied depending on population, location, and trauma specifics. Demirci (2018) focused on comparing individuals diagnosed with and without psychiatric, metabolic, or neurological conditions. Fontes et al. (2017), Schneiderman et al. (2018), and Langevin et al. (2017) had control groups without identified trauma or abuse that were similar in age, geographic location, and/or socioeconomic status to the sample group studies. Hash et al. (2019) uniquely involved comparison of a retrospective intervention study of a caregiver home program group for infants 10-24 month old identified by Child Protective Services (CPS) to a referral and resource design control group.
4. Differences between sexes
One study demonstrated sex differences in their results (Schneiderman et al., 2018). For females, depressive and PTSD symptoms at pre-test predicted sleep disturbances at post-test and sleep disturbances at pre-test also predicted depressive and PTSD symptoms at post-test. However, no significant relationship was found for males between maltreatment and sleep disturbances nor PTSD symptoms and sleep disturbances.
5. Type of trauma
1) Childhood sexual abuse
Seven articles focused on reported Childhood Sexual Abuse (CSA) (Demirci, 2018; Fontes et al., 2017; Hébert et al., 2017; Langevin et al., 2017; Mansbach-Kleinfeld et al., 2015; Melville et al., 2014; Mignot et al., 2018). CSA occurs when a child is coerced into sexual activity (American Psychological Association, n.d.). Examples of sexual activity include kissing, promiscuous touching, digital or penile penetration, and exposure of a minor to pornography (American Psychological Association, n.d.). Statistics on CSA range widely. Studies have shown that 11-53% of girls and 4-60% of boys worldwide experience CSA before their 18th birthday (Melville et al., 2014). This variation exists because the definition of CSA differs according to geographic location (Cohen, 2007). For example, some countries base their definitions of CSA solely on sexual physical contact; whereas, other countries define CSA based on physical contact and non-physical forms of sexual abuse.
2) Trauma related to caregiver events
Trauma related to caregiver events was addressed by one study, which evaluated the effects of nine different ACEs on young children, 10-24 months old, who were recruited from CPS (Hash et al., 2019). The most commonly identified ACE stemmed from caregiver mental illness and caregiver divorce/separation for both a home visitation parent-relationship intervention called, Promoting First Relationships (PFR), and a Resource-Referral Service (RRS). Trauma induced by caregiver mental illness was present in about 50% of participants within each intervention group (57.3% PFR, 55.3% RRS), while trauma from caregiver divorce/separation was an issue for less than half of the children within the same intervention groups (39.5% PFR, 41.5% RRS).
3) Maltreatment types
ACEs related to maltreatment were examined in 5 of the 14 articles (McPhie et al., 2014; Okada et al., 2018; Schneiderman et al., 2018, Wang et al., 2016; Yen at al., 2015). McPhie et al. (2014) found that 78.1% of the youth sample involved with CPS experienced one or more types of maltreatment, surpassing the clinical severity cutoff, with physical abuse being the most frequently reported type. Okada et al. (2018) specified psychological abuse (53.1% of children who had experienced abuse) as the highest type of adverse condition experienced by participants. In the Schneiderman et al. (2018) (55.8% of maltreated participants) study, the most pronounced form of maltreatment was neglect. Wang et al. (2016) studied childhood trauma with a list of 18 potentially traumatic events. They discovered that interpersonal violence had the greatest impact on insomnia, while rape had the greatest risk relative to all other 17 adversities. Yen et al. (2015) examined abuse in the form of bullying in the school setting and found that bully victims experienced the highest percentage of physical abuse (25.7%), followed by teacher harassment (21.2%). Hambrick et al. (2018) concentrated on ACEs but generalized the types of ACEs experienced, so the specific ACEs experienced with study participants could not be determined. Finally, two of the articles demonstrated a doseresponse to sleep and ACEs, in which, as the number of traumatic experiences increased, sleep disturbances likewise increased (Hash et al., 2014; Wang et al., 2016).
6. Outcome measures
1) Self-reported vs. Caregiver-reported
Sleep was measured using both formal and informal assessments. Nine of the studies included sleep outcome measures that were self-reported (Demirci, 2018; Fontes et al., 2017; Mansbach- Kleinfeld et al., 2015; McPhie et al., 2014; Melville et al., 2014; Mignot et al., 2018; Okada et al., 2018; Schneiderman et al., 2018; Yen et al., 2015). Four of the studies used assessments that were answered by a caregiver or professional who knew the child well (Hambrick et al., 2018; Hash et al., 2019; Hébert et al., 2017; Langevin et al., 2017;. Wang et al. (2016) did not assess sleep with a formal questionnaire but did face-to-face interviews.
2) Formal sleep assessments
Five studies employed formal sleep assessments. Demirci (2018) and Schneiderman et al. (2018) used the Pittsburgh Sleep Quality Index (PSQI) to capture overall sleep quality scores. In addition to the PSQI, Demirci (2018) administered the Insomnia Severity Index for more detailed data on insomnia symptoms. Hash et al. (2019) utilized a modified version of the Brief Infant Sleep Questionnaire, asking only one of the assessment questions to parents, “Do you consider your child’s sleep as a problem?” The study authors elected to use only one of the questionnaire items because evidence indicated that symptoms of common sleep problems in children age 0-2 years is significantly connected to parent responses on their perception of their child’s sleep quality. Okada et al. (2018) used the Brief Sleep Questionnaire, a 19-item assessment designed for children aged 6-12 years. The Brief Sleep Questionnaire evaluates how often a child experiences symptoms related to bedtime, sleep, waking, and daytime sleepiness. Three studies used the Child Behavior Checklist, which includes a 7-item sleep subtest (α=0.82), accepted as a formal assessment of sleep in practice (Hambrick et al., 2018; Hébert et al., 2017; Langevin et al., 2017). Yen et al. (2015) captured subjective severity of insomnia symptoms and sleep related distress exhibited by participants using the Taiwanese version of the 8-item Athens Insomnia Scale (AIS-8). Assessments Not Specific for Sleep Quality
The following outcome measures focused on adolescent trauma but did not include sleep specific assessments in the study design. Instead, sleep was assessed as a sub-category in an informal assessment. Melville et al. (2014) created a child psychosocial assessment tool that included questions about night time wakings, nightmares, and difficulty falling asleep. Mansbach-Kleinfeld et al. (2015) asked about physical symptoms and body image variables. Sleep disturbance was measured by asking if the adolescent had “difficulty falling asleep in the past 6 months.”
Fontes et al. (2017) and Wang et al. (2016) explored trauma retrospectively with national surveys that were not specific to sleep but included sleep questions. Wang et al. (2016) used the National Comorbidity Survey Replication Adolescent Supplement (NCS-A) that asked adolescents four sleep questions through a face-to-face interview. Fontes et al. (2017) included a single-item insomnia variable [1 (the student always or almost always has sleep problems) or 0 (student never has any sleep problems)] included in the National School Health Survey-Pesquisa Nacional de Saúde do Escolar (2015 PeNSE), which looked at overall health of teenagers in Brazil. See Table 6 for specific values from outcome measure results.
7. Description of sleep problems
Descriptions of sleep quality were dependent on the outcome measure used. Langevin et al. (2017), Melville et al. (2014), and Mignot et al. (2018) collected similar data on sleep problems, i.e. frequent night wakings, difficulty falling asleep, and experience of nightmares. Additionally, four different studies explored the severity of participants’ insomnia symptoms (Demirci, 2018; Mignot et al., 2018; Wang et al., 2016; Yen et al., 2015).
Schneiderman et al. (2018) described the only study that specifically used the verbiage, “sleep disturbances.” Mignot et al. (2018) classified sleep problems as “awakening too early in the morning” and as sleep being “not satisfactory.” Langevin et al. (2017) and Okada et al. (2018) took a more in-depth look at sleep quality questions. For example, Langevin et al. (2017) asked participants if they did “not want to sleep alone,” did “not want to sleep at night,” slept “less than most children in the day or night,” and “talked or screamed in their sleep.” Okada et al. (2018) asked about specific issues, such as “bedtime and waking symptoms,” “sleeping symptoms,” “daytime sleepiness,” “some form of suspected sleep disorder,” “difficulty getting out of bed in the morning,” “poor waking habits,” “fear of sleeping in the dark,” “wakes up in a negative mood,” “resists going to bed at bedtime,” and “needs special object to fall asleep.”
Ⅳ. Discussion
Addressing problems with sleep is a developing area of practice in occupational therapy. Although occupational therapy research has addressed the impact of sleep disturbance in children with ADHD and autism spectrum disorder (Ismael, Lawson, & Hartwell, 2018; Koenig & Rudney, 2010; Vasak et al., 2015), the profession has done little research on the impact of sleep disturbance with identified ACEs during childhood. The present study sought to expand the understanding of how trauma affects a child’s sleep participation to more clearly define the role of occupational therapy in addressing this issue.
The ACEs investigated in this study included child neglect, physical/emotional abuse, child sexual abuse, caregiver mental illness, caregiver incarceration, and exposure to violence. The current review demonstrates moderate evidence indicating that childhood abuse is related to sleep quality. It specifically looked at sleep problems in children to better understand if and when sleep is impacted and found a consistent association between childhood sleep disturbances and trauma for children from as young as 10 months to as old as 18 years.
Schneiderman et al. (2018) found that maltreatment did not significantly increase sleep disturbances for males. The authors explained the unexpected finding by attributing the phenomenon to concurrent exposure of experimental groups to contextual factors, such as loud traffic noise. Adolescents with identified trauma were compared to peers living in corresponding low-income, urban zip codes with similar environmental structures. Thus, the control and maltreatment groups potentially experienced similar sleep quality issues due to exposure to non-ideal sleep environments, resulting in no significant difference between the groups’ sleep quality. These findings may also indicate potential differences between sexes in sleep duration issues related to maltreatment.
The findings of this review and the pervasiveness of abuse discussed throughout the literature bolster the argument for occupational therapy research and clinical practice to more intentionally address the topic of children’s sleep, specifically with children who have experienced ACEs. The results of this review, informed by other recent literature, suggest a need for the implementation of routine sleep assessments and sleep interventions in the pediatric therapy setting. Such sleep assessments and interventions can serve as valuable strategies for early intervention to prevent the known outcomes of poor sleep, such as impaired academic performance and elevated disease risk. This review demonstrated that trauma affects sleep in individuals as early as 10 months old.
1. Strengths and limitations
This review summarizes the body of literature examining the relationship between sleep and trauma in children from infancy to adolescence. The study populations represent a large number of participants and almost all continents, suggesting a wide applicability of the results. Findings from these studies indicate negative effects of trauma on sleep. A majority of the included articles contained large sample sizes and relatively equal gender ratios, supporting generalizability of the results. Regarding differences among the studies, participant origin varied greatly. Despite participant differences, the studies yielded similar results.
The diversity of the assessment tools used across articles prevented a meta-analysis of the results. Another caution for interpreting the results of this review is consideration of the potential high risk of bias in a few of the contributing studies as explained in the results section (Hash et al., 2019; Hébert et al., 2017; Langevin et al., 2017).
2. Implications for occupational therapy education
Knowing that sleep is a part of the occupational therapy domain and imperative for optimal occupational performance, occupational therapy curricula should include content:
•Acknowledging the connections between ACEs and sleep problems in the pediatric population,
•Instructing students on assessments and evaluations available to identify sleep problems, and
•Exposing students to appropriate interventions to help bridge the gap between clinical practice and the existence of poor sleep participation in children with trauma.
Furthermore, psychosocial training should be available for students and practitioners to enhance their ability to address the emotional and psychological aspects of disturbed sleep and improve outcomes for children with ACEs.
3. Implications for occupational therapy research
This review took a wide view of the relationship between trauma and sleep, examining studies across the age span of childhood and generally not differentiated by sex. It would be helpful for researchers to further examine potential differences in the relationship between trauma and sleep by age group and sex in consideration of the differences in sleep patterns across ages and sex differences found by Schneiderman et al. (2018). More studies are especially needed to examine the impact of trauma on sleep in infants. Only one of the included studies looked at sleep quality in infants, 10-24 months of age (Hash et al., 2019), while one fourth of minors with identified trauma in the U.S. is found among children 0-3 years old (U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau, 2019). Future research is needed to expand understanding of the relationship between infant sleep and trauma with appropriate interventions. The findings from this review illustrate that sleep disturbance associated with trauma emerge in the earliest stages of life and identifying those disturbances as early as possible can decrease later developmental delays that interfere with quality of life.
Researchers should also strive to expand understanding of how occupational therapy can address improving sleep outcomes for children. Since children with CSA were found to be the most prevalent in the literature, future studies should involve randomized control trials that investigate appropriate interventions for children with CSA to improve sleep outcomes and overall performance outcomes. Aside from intervention studies, future research should involve development of assessments that demonstrate sensitivity to whether a child has exposure to ACEs and experiences poor sleep participation. Such assessments would benefit clinicians in treating clients more holistically and maximizing their performance outcomes.
4. Implications for occupational therapy practice
The results of this review with consideration of other recent literature have the following implications for occupational therapy practice:
•The current evidence supports the notion that sleep problems are more prevalent in children who have experienced trauma.
•Occupational therapy practitioners should be vigilant of sleep disturbance in children and incorporate routine evaluation regarding sleep quality to practice more comprehensive care, treating infants to adolescents.
•Occupational therapy practitioners should consider incorporation of treatment for sleep disturbances in children to improve client quality of life.
Ⅴ. Conclusion
Adverse Childhood Experiences (ACEs) are common among the pediatric population. This study performed an exhaustive systematic search of the literature to find general agreement that ACEs are associated with sleep problems in children. Because sleep is included in the domain of occupational therapy, future research is needed to develop effective and appropriate occupational therapy interventions for sleep disturbances in children with traumatic experiences. A desired outcome of this review was to encourage occupational therapists to contribute to the emerging understanding about sleep science by (1) understand the need for more evidence-based interventions that improve quality of life for children with sleep disorders, (2) increase their awareness of the relationship between occupational performance and sleep disturbances related to ACEs, and (3) regularly incorporate sleep assessments in initial evaluations and sleep interventions into treatment plans for children who have experienced ACEs.